Is Infrared Thermography Reliable to Assess Pain in the Trapezius Muscle Region?
Abstract
Objective:
The aim of this study was to evaluate the inter- and intra-examiner reliability of infrared thermography (IT) in skin temperature analysis of people with pain complaints in the upper trapezius muscle.
Methods:
A total of 82 subjects (24.8 ± 6.9 years; 63.8 ± 13.1 kg) of both genders who had moderate (VAS-3) or severe pain in the upper trapezius muscle were evaluated. Skin temperatures of four areas (ROIs) were analyzed by IT using a FLIR camera (model T640SC - Sweden). Each evaluator performed two area analyses at different times.
Results:
The evaluation of the four areas indicated a very strong overall intraclass correlation coefficient (ICC) for both intra-examiner (Examiner 1: ICC = 0.936; 95% CI = 0.905–0.959; P < 0.001; Examiner 2: ICC = 0.979; 95% CI = 0.968–0.987; P < 0.001) and inter-examiner (Measurement 1: ICC = 0.933; 95% CI = 0.902–0.958; P < 0.001; Measurement 2: ICC = 0.979; 95% CI = 0.968–0.987; P < 0.001). The ICC was regular on ROI 3 in the measurement 1 inter-exam test, and the ROI 1, ROI 2, and ROI 4 values were strong; all points were very strong in measurement 2. The ICC was rated from strong to very strong for both examiners in the intra-examiner test at all points.
Conclusion:
IT was reproducible in measuring the upper trapezius muscle skin temperature, and the intra and inter-examiner agreement levels can be used as a reliable tool in clinical practice.
1. INTRODUCTION
Infrared image analysis has the following advantages as a diagnostic aid: it is a non-invasive technique, painless, contactless, non-intrusive, no ionizing radiation, innocuous, makes surface temperatures available in real-time images, shows the location of the lesion, and is able to demonstrate metabolic and physiological changes through a functional examination rather than strictly through anatomical details as in other analysis methods [1].
Researchers interested in investigating the use of infrared thermography (IT) in healthcare [2, 3] report the benefit of the method in evaluating musculoskeletal injuries to monitor various clinical conditions. Detection of small temperature changes in specific regions may suggest changes in physiology, contributing to screening, diagnosis, follow-up, and treatment [4-6].
It is a non-invasive, contactless method used to record thermal body patterns, capturing the heat emitted by the body or parts of it. IT has been used for some years to determine changes in the musculoskeletal system, becoming a great aid in the evaluation and diagnosis processes as it provides objective parameters, in addition to having high sensitivity [7-9].
Among musculoskeletal disorders, myofascial trigger points (MTP) trigger changes in muscle activity, limit joint mobility and autonomic manifestations, and most frequently occur in the upper trapezius muscle [10-13] due to permanent activity and microtrauma in this region [14]. These changes may cause changes in the local microcirculation, affecting the skin temperature, which allows the possibility of using thermographic imaging in this analysis [15, 16].
As a means of objective assessment, measuring the skin temperature of the painful region has been shown to be a promising strategy capable of providing feedback on possible changes which are common in painful conditions, assisting in the assessment, monitoring, and results of differentiated treatments [17].
However, its applicability and effectiveness as an evaluation method need further testing because it is a new methodology in health and because there are still only a few studies on different local analysis methodologies regarding the reliability of trapezius muscle temperature assessment using thermographic imaging [15, 16, 18]. Thus, considering the hypothesis that IT is a reliable and reproducible measurement, the objective of the present study was to evaluate the intra and inter-examiner reliability of IT in skin temperature analysis in people with pain complaints in the upper trapezius muscle.
2. MATERIALS AND METHODS
2.1. Participants
A total of 87 individuals were initially selected for the study; however, 5 were not included in the final sample because they did not meet all the necessary criteria. Thus, the sample consisted of 82 subjects (24.8 ± 6.9 years; 63.8 ± 13.1 kg; 1.65 ± 0.09 m; body mass index (BMI) = 23.3 ± 3.6 kg/m2) of both genders with pain complaints in the upper trapezius muscle and meeting the following inclusion criteria: minimum age of 18 years, both genders, and moderate pain level (≥3 points) on the visual analog scale (VAS) in the upper trapezius muscle. The participants did not present coagulation dysfunctions, fibromyalgia, cervical radiculopathy, no head/neck/shoulder girdle surgeries, or were not undergoing any anti-inflammatory/acupuncture/muscle relaxant treatment upon clinical examination. The exclusion criteria were as follows: fever, VAS < 3 points, or withdrawal from participating in the study.
This study was part of a larger project titled “Using Thermography as a Relevant Method in Diagnosing Trigger Points and Evaluating Therapeutic Techniques,” approved by the Ethics Committee for Research on Human Beings of the Federal University of Sergipe (CEP/UFS), Opinion No. 2,897,511/2018 and CAAE: 74397517.6.0000.5546, and submitted to the Brazilian Registry of Clinical Trials platform (ReBEC): RBR-6p4jnf. All participants signed informed consent forms prior to participating in the study.
The adopted procedures followed the standards of ethics in research with human beings according to resolution No. 466 of 12/12/2012, which are the guidelines and regulatory standards for research involving human beings, and in accordance with the ethical principles contained in the Declaration of Helsinki (1964), reformulated in 1975, 1983, 1989, 1996, 2000, 2008 and 2013) of the World Medical Association.
2.2. Procedures and Thermographic Registration
Subjects were instructed not to touch, press, rub, or scratch their skin over the upper trapezius muscle at any time prior to the examination; not to take any medicines which may be temporarily suspended; not to ingest thermogenic products within two hours of the examination; not to apply moisturizer, lotion, oil, etc., on the skin [19, 20].
Skin temperature was assessed by thermographic imaging using a FLIR camera (model T640SC - Sweden) operating at a frequency of 30 Hz, thermal sensitivity of 0.02° C, resolution of 640 x 480 pixels and a spectral range of 7–13 µm, in a range of images with temperatures between 20 and 120° C, with ± 2% accuracy.
The thermographic image capture was performed in a climate-controlled room with a temperature between 22ºC and 23ºC, where the subjects remained for 10 minutes so that they could reach thermal equilibrium before the image acquisition process. All of the subjects remained standing and dressed only in underwear (shorts, bikini, or swimsuit) during the exam. The camera was fixed on a tripod at a distance of one meter from the subject sitting in a chair. The framed region (upper trapezius muscle) and the height adjustment of the camera depended on the height of the subject. All photographic records were taken by a single observer who was familiar with the camera and the technique [4, 9, 21].
2.3. Infrared Thermography Reliability
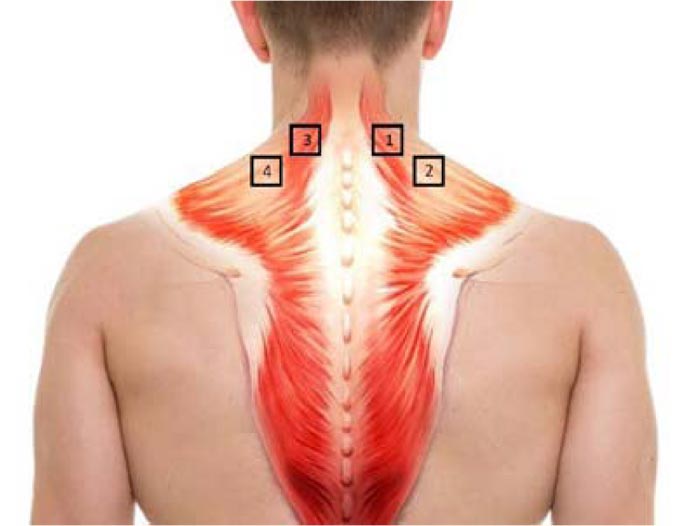
A posterior trunk image was used for the intra-examiner reliability analysis, in which the four regions of interests (ROIs) were delimited with adhesive tape, as illustrated in (Fig. 1). The evaluators analyzed the images on two different days. The first evaluation was done on the day the images were taken using the thermographic camera, and the second evaluation was done 10 days later. The analyses used the FLIR Systems software program (version 1.1).
The inter-examiner reliability assessment was performed between two evaluators, both with minimal experience in analyzing at least 100 thermographic images in different locations so that there was no exchange of information between them on data comparison during the analysis.
2.4. Statistical Analysis
The Statistical Package for Social Sciences software program (version 22.0) was used for data processing and analysis. The intraclass correlation coefficient (ICC) was used for the intra-examiner agreement analysis using the mean and 95% confidence interval, obtaining the complete agreement of the two-moment comparison (two-way mixed). ICC was also used in the inter-examiner analysis with the average measurements and a 95% confidence interval, and complete agreement between the two evaluators (two-way randomized) was reached.
The interpretation of the reliability and reproducibility of the data were according to Callegari-Jacques [22] and Cohen [23, 24], and the interpretation of the magnitude of the agreement estimators (ICC) met the following classification: null = 0.0; weak = 0.01 to 0.3; regular = 0.31 to 0.6; strong = 0.61 to 0.9; very strong = 0.91 to 0.99; and full = 1.0. A p-value of < 0.05 was used to identify the significance of the correlation in all tests.
3. RESULTS
(Tables 1, 2, and 3) show the ICC results for the inter and intra-rater general agreement analysis of the four areas analyzed.
The four-point assessment indicated a very strong overall intraclass correlation coefficient for both the intra-examiner test (Examiner 1: ICC = 0.960; 95% CI = 0.946–0.972; P < 0.001; Examiner 2: ICC = 0.993; 95% CI = 0.976–0.988; P < 0.001) and for the inter-examiner test (Measurement 1: ICC = 0.958; 95% CI = 0.943–0.971; P < 0.001; Measurement 2: ICC = 0.982; 95% CI = 0.976-0.988; P < 0.001), indicating excellent agreement between measurements, showing very strong reliability (Table 1).
Reliability tests by ROI showed a strong correlation (ICC: 0.825–0.839) for intra-examiner assessment, considering the good agreement between the two measurements on examiner 1’s ROIs 2, 3, and 4, and very strong (ICC: 0.904–0.992) for the ROI 1 measurements of the first examiner and all trigger points analyzed of the second examiner (Table 2).
| Intraexaminer | Measurement 1 | Measurement 2 | CI: 95% | ICC | P |
| Examiner 1 | 32.79 (1.38) | 32.78 (1.40) | 0.946-0.972 | 0.960 | < 0.001 |
| Examiner 2 | 32.81 (1.40) | 32.84 (1.37) | 0.976-0.988 | 0.983 | <0.001 |
| Intraexaminer | Examiner 1 | Examiner 2 | CI: 95% | ICC | P |
| Measurement 1 | 32.79 (1.38) | 32.81 (1.40) | 0.943-0.971 | 0.958 | < 0.001 |
| Measurement 2 | 32.78 (1.40) | 32.84 (1.37) | 0.976-0.988 | 0.982 | <0.001 |
| ROI | Measurement 1 | Measurement 2 | CI: 95% | ICC | P |
|---|---|---|---|---|---|
| Examiner 1 | |||||
| 1 | 33.14 (1.30) | 33.12 (1.31) | 0.852-0.938 | 0.904 | < 0.001 |
| 2 | 32.46 (1.42) | 32.44 (1.39) | 0.741-0.892 | 0.833 | < 0.001 |
| 3 | 32.86 (1.52) | 32.90 (1.57) | 0.728-0.887 | 0.825 | < 0.001 |
| 4 | 32.49 (1.40) | 32.46 (1.40) | 0.750-0.896 | 0.839 | < 0.001 |
| Examiner 2 | |||||
| 1 | 33.09 (1.32) | 33.15 (1.20) | 0.964-0.985 | 0.977 | < 0.001 |
| 2 | 32.47 (1.39) | 32.52 (1.37) | 0.988-0.995 | 0.992 | < 0.001 |
| 3 | 32.78 (1.64) | 32.82 (1.55) | 0.959-0.983 | 0.974 | < 0.001 |
| 4 | 32.51 (1.36) | 32.48 (1.36) | 0.979-0.991 | 0.987 | < 0.001 |
The agreement for the inter-examiner evaluation in the first measurement was strong (ICC: 0.775–0.881) for all ROIs. The agreement was very strong for the second measurement (ICC: 0.958–0.985) in all ROIs (Table 3).
| ROI | Examiner 1 | Examiner 2 | CI: 95% | ICC | P |
|---|---|---|---|---|---|
| Measurement 1 | |||||
| 1 | 33.14 (1.30) | 33.09 (1.32) | 0.815-0.923 | 0.881 | < 0.001 |
| 2 | 32.46 (1.42) | 32.47 (1.39) | 0.724-0.885 | 0.822 | < 0.001 |
| 3 | 32.86 (1.52) | 32.78 (1.64) | 0.652-0.855 | 0.775 | < 0.001 |
| 4 | 32.49 (1.40) | 32.51 (1.36) | 0.751-0.896 | 0.839 | < 0.001 |
| Measurement 2 | |||||
| 1 | 33.12 (1.31) | 33.15 (1.20) | 0.935-0.973 | 0.958 | < 0.001 |
| 2 | 32.44 (1.39) | 32.52 (1.37) | 0.973-0.989 | 0.983 | < 0.001 |
| 3 | 32.90 (1.57) | 32.82 (1.55) | 0.947-0.978 | 0.966 | < 0.001 |
| 4 | 32.46 (1.40) | 32.48 (1.36) | 0.976-0.990 | 0.985 | < 0.001 |
4. DISCUSSION
The present study showed that the IT of the ROIs in the upper trapezius muscle region demonstrated recommended reliability for clinical evaluation and research, presenting strong and very strong ICC values for both intra and inter-examiner in the absolute majority of the measurements.
Therefore, IT presented a very strong general ICC for both the intra-examiner and inter-examiner tests in evaluating the four points indicated. The point by point intra-examiner evaluation showed a very strong correlation for ROI 1 measurements and strong in ROIs 2, 3, and 4, with good agreement by examiner 1; in addition, there was a very strong correlation for both measurements at all trigger points analyzed for examiner 2. The first measurement agreement in the inter-examiner evaluation was strong in all ROIs. Agreement in the second measurement was very strong in all MTPs (Table 3).
Infrared thermography (IT) is a non-invasive and non-radioactive technique capable of analyzing physiological functions related to the control of skin temperature and constitutes a possible method for identifying TPs (trigger points), as it considers the metabolic and vasomotor changes that these points cause on the fabric. It can also be useful in monitoring the evolution of TPs, comparing the thermal changes of the skin at and near the region where the palpation identified the nodules because the autonomic nervous system and the local microcirculation activities are affected by the aggravation of these points and the IT can measure the minimum temperature variations radiated by them [25, 27].
According to Silva et al. [28], reliability and agreement studies provide information for good clinical evaluation and can monitor the treatments of various diseases. IT can be used as an assessment tool in physical therapy practice because trigger point physiology is directly linked to blood circulation [28]. The results of the present study corroborate those by Dibai-Filho et al [25], in which the reliability for both intra-examiner and inter-examiner was excellent, with ICC values ranging from 0.908 to 0.993 for evaluating the upper trapezius trigger points with the use of IT.
A study by Costa et al [16] analyzed skin temperature through IT and showed excellent intra- and inter-examiner reliability for point and linear analyses on the following muscle MTPs: masseter, anterior temporal, suprahyoid, and upper trapezius. In studies by Petrova et al [29] and Antonaci et al [8], the ICC values found in the MTPs evaluation ranged from 0.60 to 0.97, being compatible with the values of the current study in which the ICC ranged from 0.657 to 0.989 in the intra-examiner comparison and from 0.579 to 0.979 in the inter-examiner comparison.
According to Nascimento et al [18], this ICC variation from 0.64 is equivalent to a ratio between the number of agreement evaluations and the number of subjects greater than 70%, considered relevant for clinical studies. A study by Silva et al [28] evaluated the intra and inter-examiner reliability of IT images for analyzing the plantar surface of people with diabetes mellitus at 18 predetermined points and showed a strong correlation (ICC:> 0.75; 95%, IC > 0.70; P < 0.01), as in the present study, reinforcing the use of IT as a reliable evaluation method to measure an increase or decrease in skin temperature arising from inflammation of local or systemic origin.
Some researchers have reported [30-32] that the use of IT as a method in evaluating musculoskeletal disorders has been useful to assist in the diagnosis and monitoring of various conditions, where the detection of small changes in temperature in specific regions of the body may suggest changes in the physiology. Thus, it is recognized as a viable method for monitoring and evaluating interventions in individuals with MTPs (muscle trigger points) [25, 33].
This study was limited by an inter-examiner analysis with only two examiners. Further studies are suggested to demonstrate the reliability and reproducibility of thermographic image analysis among a larger number of examiners in different body regions.
CONCLUSION
The results of the present study demonstrate that evaluating the skin temperature in upper trapezius muscle trigger points by IT is reliable, with a good agreement in both intra-examiner and inter-examiner tests, proposing that it is a scientifically viable method as it has excellent reproducibility for research or clinical studies in health.
LIST OF ABBREVIATIONS
| IT | = Infrared Thermography |
| MTP | = Myofascial Trigger Points |
| BMI | = Body Mass Index |
| VAS | = Visual Analog Scale |
| ROI | = Region of Interest |
| ICC | = Intraclass Correlation Coefficient |
| TPs | = Trigger Points |
ETHICAL APPROVAL AND INFORMED CONSENT
This study was approved by the Ethics Committee for Research on Human Beings of the Federal University of Sergipe (CEP/UFS), Brazil. Opinion No. 2,897,511/2018 and CAAE: 74397517.6.0000.5546.
HUMAN AND ANIMALS RIGHTS
No animals were used in this study. Reported experiments on humans were in accordance with the ethical standards of the committee responsible for human experimentation (institutional national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
All participants signed informed consent prior to participating in the study.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflicts of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


