Efficacy of McKenzie Manipulative Therapy on Pain, Functional Activity and Disability for Lumbar Disc Herniation
Abstract
Introduction:
Lumbar disc herniation (LDH) is a common determinant of low back pain (LBP) and priority for cost-effective therapeutic approach is necessary. The objective of the study was to explore the effectiveness of McKenzie Manipulative Therapy (MMT) for patients with LDH.
Methodology:
This was an assessor blinded, 36-month RCT, at Center for Rehabilitation of the Paralyzed (CRP) in Savaar, Bangladesh. Seventy-two subjects, ages 28-47 years and clinically diagnosed with MRI findings of LDH, were randomly recruited from hospital records and sixty-eight found eligible. The control group received stretching exercise and graded oscillatory mobilization, and the experimental group received McKenzie manipulative therapy for 12 sessions in 4 weeks, both groups received a standard set of care also. The pain was the primary outcome and the secondary outcome was participation in functional activities and disability.
Results:
Pain and Disability found significant improvement in both groups, with the McKenzie approach significantly superior to the control group (p<.05). Bothersome in Activities (SBI) reported significantly lower post report compared to baseline for both groups (p<.01). McKenzie showed significantly superior outcomes for fear avoidance (FABQ) total and SBI feeling of abnormal sensation in leg compared to the control group (p <.05).
Conclusion:
The McKenzie manipulative therapy approach was found to be effective for pain, disability and participation in activities for single or multiple level LDH patients in a short time from day 1 to week 4, and the treatment effect extends after 6 months.
Clinical Trial Registration No.: CTRI/2020/ 04/024667.
1. INTRODUCTION
In developed countries, more than 80% of the population is affected by low back pain (LBP) at some time in their life [1, 2]. The international prevalence of low back pain has been reported between 49 to 80% [3]; Thirty-one studies have reported the prevalence of back pain in India varies from 62% in the general population to 78%, with Lumbar disc herniation (LDH) is one of the prominent causes of low back pain [4]. LDH is defined as the localized displacement or disruption of disc material beyond the margins of the intervertebral disc space, is considered to be the most common cause of lumbosacral radiculopathy [5]. The severity of symptoms depends upon the level of disc displacement compressing the posterior or postero-lateral aspect of Lumbar spinal segments. LDH causes central low back pain and/ or radiating pain over the area of the buttocks or legs served by one or more spinal nerve roots of the lumbar vertebrae or sacrum, combined with neurologic deficits or associated symptoms of nerve root compression [6, 7]; the phenomenon can also lead to motor deficits of lumbosacral plexus, impairments in regular functions related to activities and livelihood [7].
LDH is one of the most common problems confronting outpatient physical therapists. It is extensively established that herniation is a multidimensional mechanical disorder that is dependent on physical factors, lifestyle, and psychosocial factors [8]. The management of LDH depends on the severity of disc displacing, causing a spectrum of clinical presentations [9] and a conservative treatment approach is recommended for the patients without red flags. The red flag indicates extreme pain, progressive neurological deficit, and/or cauda equine syndrome. Conservative care includes a variety of pharma- ceutical and non-pharmaceutical treatments such as patient education, analgesics, rest, exercise, traction, manipulation, mobilization, manipulative therapies; clinical guideline [10] suggests prioritizing conventional therapy as the first line of management although surgical or invasive therapies can be the treatment of choice [11, 12].
The McKenzie method is widely prescribed by physical therapists to treat pain and increase flexibility for the patients having definite mechanical characteristics of LDH symptoms [13, 14]. McKenzie Mechanical Diagnosis and therapy combine exercise based on directional preferences that are intended to “reduce derangements” and typically demonstrates one direction of repeated movement which decreases or centralizes referred symptoms, abolishes midline symptoms and emphasizes self-directed exercises performed by patients with manipulative therapy approach by the clinician [15]. McKenzie's approach is evident to be effective for low back pain in contrast with pain and disability in the short term and long term and considered as cost-effective. Hence, this is a research gap on specific concentration to lumbar disc herniation to evaluate if McKenzie manipulative therapy is effective [15, 16]. Also, there are recommendations for evaluating the therapeutic approach for low-resource countries [16]. The study is intended to report the effectiveness of McKenzie manipulative approach for LDH patients compared to stretching and conventional manipulative therapy approach regarding outcomes of : (1) pain in different functional positions, (2) fear avoidance behavior,(3) Bothersome in functional activities and (4) low back disability index.
2. METHODS
The study was an assessor-blinded, randomized clinical trial (RCT), and carried out for 36 months at the Centre for the Rehabilitation of the Paralysed (CRP) in Bangladesh. The study was approved by the CRP ethical review board (CRP-R&E-0401-180). The study is a fundamental feasibility study of the research project titled “Manipulative therapy for Prolapsed lumbar Intervertebral disc (PLID) patients and relation with infectious diseases: A Randomized Controlled Trial” approved by Clinical trial registry India (CTRI/2020/ 04/024667) the primary registry authority approved by WHO trial registry.
2.1. Patients, Sample Size Calculation and Randomization
From June 2017 to December 2019, 72 patients aged 25- 50 years with a complaint of low back pain and/or radiating pain and /or neurological symptoms towards lower limbs have been primarily enrolled in the study. Then they were investigated as per inclusion criteria (diagnostic criteria). Persons having MRI and previously diagnosed as Disc herniation or Lumbar disc herniation LDH or Prolapsed Lumbar intervertebral disc (PLID) were also enrolled and screened for the second time; the persons who had no MRI were advised to perform with proper justification. Samples were enrolled in the study through hospital randomization and voluntary participation. Sixty-eight (n=68) patients complied with the eligibility criteria and were assigned after voluntary written consent, Calculated according to Miot [17]. Subjects were randomized either into the McKenzie group or conventional physiotherapy group with computer-generated, concealed allocation. The inclusion criteria were : (1) patients with a single or multiple levels of lumbar disc herniation evident in Magnetic Resonance Imaging MRI, (2) positive Lasègue's sign or cross Lasègue's sign and (3) diagnosed as derangement syndrome 1-3 in Mechanical Diagnosis and Therapy -MDT assessment by McKenzie institute. The exclusion criteria were (1) any history of surgery for LDH, : (2) co-morbidity associated with endocrine disease, osteopenia, infection or carcinoma, (3) History of fracture in the spine, ribs, or upper limb within last 1 year, and (4) pre-existing phobia to physiotherapy or manipulative therapy. Both groups received interventions from two outpatient settings of a hospital. Interventions were given by an experienced physiotherapist ranging from 2-10 years of clinical practice experience, and a subsequent in-service training by co-researchers for the specific treatment protocol. The single assessor was blinded to the assignment and performed all assessments. The data was taken before treatment and after 12 sessions (4 weeks) of treatment in the hospital setting; a follow up was taken after 6 months of discharge by a phone call or a physical visit.
2.2. Interventions
The experimental group received McKenzie manipulative therapy for the lumbar spine. The manipulative therapy included repeated movements, typically include flexion in lying or standing; extension in lying or standing; and lateral movements of either side gliding or rotation and manipulative approach to lumbar spine segments [18, 19]. Patients performed those movements at therapy sessions and home [20]. The repeated movements of McKenzie manipulative therapy has been prescribed as 10 repetitions of directed movements, 2-3 hourly in 14 hours of a day and for 4 weeks. Manipulative therapies were performed by physiotherapists for 10-15 repetitions in a single “on/off” maneuver for 5-7 minutes for 6 sessions in 2 weeks. The control group received manual passive stretching exercise for lumbopelvic muscles for 5-7 repetitions per muscle with 10-15 seconds hold performed twice a day for 2 weeks and graded oscillatory mobilization in Maitland concept in 5-7 minutes, 35-40 oscillation per minutes or static segmental mobilizations in Maitland concept for 35-50 second hold for 5-7 times in lumbar spine for 6 sessions in 2 weeks also, both groups received analgesics and hot compression in the lower back for 10 minutes for 2 weeks, stabilization exercises of lumbopelvic segment accompanied with a booklet indicating the proper way to do different activities and lifestyles habits for 4 weeks [21]. All of the interventions ended up after 4 weeks from the initial day of treatment.
2.3. Outcome Measurements
The pain was the primary outcome and the secondary outcome was participation in functional activities and disability. The pain was measured by the Dallas pain questionnaire (DPQ) in different activities and positions. Participation in functional activities was measured by the Fear-avoidance beliefs questionnaire (FABQ) and Sciatica Bothersome Scale (SBS) and disability was assessed with the Oswestry Low Back Disability Questionnaire (ODI). All outcome measurement tools were found to have satisfactory sensitivity and reliability [22-26]. The outcomes were measured before intervention (day 1) and after 12 sessions (4 weeks) of intervention in the rehabilitation center setting for all the variables. A follow up was measured 6 months after discharge by a phone call or a physical visit through DPQ and ODI.
2.4. Statistical Analysis
Data entry and checking the quality of data was examined by an independent non-associated researcher. Data were obtained in a general linear model for paired and independent t-test, and Mixed ANOVA Repeated Measures in SPSS Version 20. DPQ and ODI were analyzed utilizing a paired and independent t-test for time fraction analysis and Repeated Measures ANOVA for repeated measure analysis. FABQ and SBS were analyzed utilizing a paired t-test for within-group measures and independent t-test compared to baseline with a 5% level of significance. The chi-square test and independent-samples t-test were used to compare and determine the similarities of clinical baseline characteristics between the groups.
3. RESULTS
3.1. Socio-demographic Data
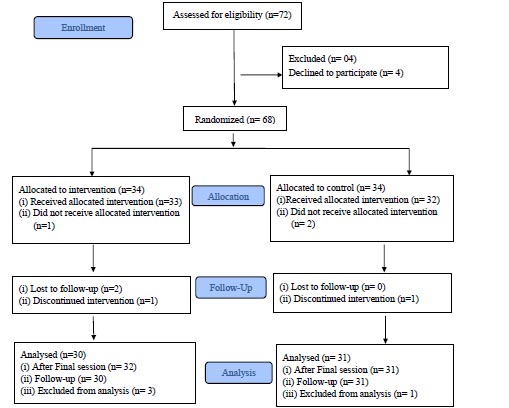
Sixty-eight (n=68) respondents were enrolled and randomly selected for each group. Within the control group, 3 subjects dropped out and the experimental group reported 4 subjects withdrew from the study (Fig. 1). In baseline assessment (Table 1), the control group reported a mean age, height, and weight as 38.59 ± 10.891 years, 61.38± 5.205 inches, and 63.97± 8.959 Kg; and the experimental group reported age at37.71± 8.803 years, 60.50 ± 5.160 inches, and 64.06± 8.180 Kg respectively. As both groups had a similar number of respondents, their occupations with service holder (Control n=7, Experimental n=8) and housewife (Control n= 7, Experimental n=9) comprising the majority of respondents. The level of the disc herniation evident from MRI readings was reported as follows: L4/5 (Control n= 9, Experimental n=8), L5/S1 (Control n= 8, Experimental n=9), and more than one level (Control n= 14, Experimental n=13). There were no significant differences in baseline characteristics between groups.
| - | Control group (Mean ± SD) |
Experimental group (Mean ± SD) |
p |
|---|---|---|---|
| Mean age (years) | 38.59 ± 10.891 | 37.71± 8.803 | 0.714 1 |
| Sex (Male/Female) | (24/10) | (21/13) | 0.442 2 |
| Mean Height (inches) | 61.38± 5.205 | 60.50 ± 5.160 | 0.485 1 |
| Mean Weight (kg) | 63.97± 8.959 | 64.06± 8.180 | 0.966 1 |
| Occupation | |||
| Farmer | 3 | 2 | 0.998 2 |
| Daily labor | 2 | 2 | |
| Service holder | 7 | 8 | |
| Garments worker | 1 | 2 | |
| Driver | 3 | 2 | |
| Businessman | 6 | 5 | |
| Unemployment | 1 | 1 | |
| Housewife | 7 | 9 | |
| Teacher | 3 | 2 | |
| Student | 1 | 1 | |
| Level of herniation | |||
| L2/3 | 1 | 2 | 0.975 2 |
| L3/4 | 2 | 2 | |
| L4/5 | 9 | 8 | |
| L5/S1 | 8 | 9 | |
| More than 1 site | 14 | 13 | |
3.2. Pain and Disability
Analysis of the Dallas Pain Questionnaire (DPQ) and Oswestry Disability Index (ODI)was analyzed in three distinct statistical measures. Within-group analysis of DPQ and ODI from baseline (day 1) to discharge (4 weeks) and discharge to follow up (6 months) have been conducted by paired t-test (Tables 2-3) and hereby between-group analysis calculated by independent t-test (Tables 2-3). Changes in repeated measure from baseline (day 1) to follow up calculated with a Repeated Measures ANOVA (Table 4). Excluding the drop-out data, both the control and experimental group had significant changes separately (P=<.05) in all the variables.
3.3. Baseline (day 1) to Discharge (4 weeks)
From baseline to discharge (Table 2) within group analysis found statistical significant changes in DPQ and ODI (p=<.05). Between group analysis found DPQ interference of lifestyle (mean difference -1.19, CI -2.4, -.33; P= <.001), Pain severity in forward bending activity (MD -.95, CI -1.88, -.02; p=<.04), Back stiffness (MD -1.19, CI -2.07, -.31; p=<.00), sit in soft arm chair (MD -1.00, CI -1.99, -.012; p=<.04) and Pain limit normal lifestyle (MD -1.58, CI -2.53, -.63; p=<.001).
| Variables | Control | McKenzie | Between group | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| m1 | 95% CI | p | m1 | 95% CI | p | MD2 | 95% CI | p | ||||
| low | up | low | up | low | up | |||||||
| DPQ | ||||||||||||
| Pain | 2.85 | 2.04 | 3.65 | .00*** | 3.77 | 2.89 | 4.65 | .00*** | -.73 | -1.5 | .13 | .09 |
| Pain at night | 2.41 | 1.48 | 3.35 | .00*** | 4.38 | 3.56 | 5.20 | .001** | -.69 | -1.5 | .13 | .09 |
| Interfere with lifestyle | 1.58 | .87 | 2.29 | .01* | 3.78 | 2.98 | 4.58 | .001** | -1.19 | -2.04 | -.33 | .001** |
| Pain severity at forward bending activity | 2.56 | 1.88 | 3.24 | .00*** | 4.38 | 3.47 | 5.28 | .00*** | -.95 | -1.88 | -.02 | .04* |
| Back Stiffness | 2.12 | 1.30 | 2.94 | .02* | 3.23 | 2.51 | 3.96 | .00*** | -1.19 | -2.07 | -.31 | .00*** |
| Interfere with Walking | 3.10 | 2.36 | 3.84 | .00*** | 4.12 | 3.29 | 4.95 | .001** | .03 | -.82 | .90 | .93 |
| Hurt when Walking | 3.16 | 2.43 | 3.88 | .01* | 2.82 | 2.09 | 3.56 | .001** | -.14 | -.98 | .70 | .74 |
| Pain keep from standing still | 2.68 | 1.96 | 3.40 | .001** | 3.76 | 2.92 | 4.60 | .01* | .172 | -.82 | 1.17 | .73 |
| Pain keep from twisting | 2.39 | 1.57 | 3.20 | .00*** | 3.09 | 2.13 | 4.04 | .00** | -.10 | -1.06 | .84 | .82 |
| Sit in upright hard chair | 2.34 | 1.58 | 3.10 | .001** | 3.00 | 2.00 | 3.99 | .001** | -.55 | -1.57 | .47 | .28 |
| Sit in soft arm chair | 2.43 | 1.68 | 3.18 | .03* | 3.27 | 2.47 | 4.06 | .02* | -1.00 | -1.99 | -.012 | .04* |
| Pain in lying | 2.19 | 1.57 | 2.81 | .00*** | 4.23 | 3.36 | 5.11 | .001** | -.80 | -1.82 | .22 | .12 |
| Pain limit normal lifestyle | 2.25 | 1.54 | 2.97 | .001** | 4.10 | 3.39 | 4.81 | .00*** | -1.58 | -2.53 | -.63 | .001** |
| Interfere with work | 2.32 | 1.56 | 3.08 | .03* | 3.58 | 2.80 | 4.36 | .00*** | -.61 | -1.57 | .34 | .20 |
| Change of workplace | 1.65 | .77 | 2.53 | .001** | 4.08 | 3.29 | 4.87 | .001** | -.65 | -1.60 | .29 | .17 |
| ODI | 12.12 | 7.48 | 16.75 | .001** | 32.77 | 25.13 | 40.41 | .00*** | -6.79 | -11.9 | -1.67 | .10 |
3.4. Discharge (4 weeks) to follow up (6 months)
From discharge to follow-up (Table 3) experimental and control group separately found statistically significant changes in DPQ and ODI (p=<.05). Between-group analysis found DPQ Pain severity in forward bending activity (MD -.81, CI -1.55, -.06; p=<.03), Pain in lying (MD -1.03, CI -1.99, -.07; <.03), Pain limit normal lifestyle (MD -1.22, CI -2.14, -.29; <.01), Change of workplace (MD -.94, CI -1.79, -.09; p=<.03) and ODI (MD -8.13, CI -13.25, -3.01; P=<.00).
3.5. Baseline (day 1) to Follow up (6 months)
From baseline to follow-up (Table 4) there were statistical changes within-group and between-group analysis in all variables in DPQ and ODI. In the control group DPQ mean varies in all the variables separately, the lowest mean was 1.96 (hurt when walking) CI (1.41,-2.51), F= 3335.1, p=<.02, highest mean was 3.31 (sit in soft armchair), CI (2.51, 4.10), F= 257.8, P=<.01. In the control group, ODI was represented as (mean 35.5, CI 27.7, 43.3, F= 213.1, P=<.01). In the experimental group, DPQ had significant changes in all variables, the lowest mean was 1.61 (back stiffness), CI 1.03, 2.20, F= 186.1, P=<.01) and the highest mean was 2.97 (pain at night) CI 2.11, 3.83, F= 237.3, P=<.03. ODI in the experimental group had a mean 48.9, CI 41.1, 56.7. F= 107.1, P=<.001).
In between-group analysis (Table 4), DPQ had significant changes (p=<.05) with F value pain 1287.4, pain at night 494.3, interfere with lifestyle 732.4, pain severity at forward bending activity 722.1, back stiffness 437.1, interfere with walking 625.9, hurt when walking 463.0, pain from standing still 359.4, pain keep from twisting 474.9, sit in upright hard chair 577.6, sit in soft armchair 478.5, pain in lying 587.6, pain limit normal lifestyle 639.5, interfere with walking 513.9 and change of workplace 478.5 with statistical power 1. In between-group analysis, ODI had a statistically significant change with F value 287.5 (P=<.01, power 1).
| Variables | Control | McKenzie | Between group | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| m1 | 95% CI | p | m1 | 95% CI | p | MD2 | 95% CI | p | ||||
| low | up | low | up | low | up | |||||||
| DPQ | ||||||||||||
| Pain | 1.95 | 1.34 | 2.55 | .001** | 1.30 | .45 | 2.14 | .00*** | -.33 | -1.18 | .52 | .44 |
| Pain at night | .83 | .31 | 1.35 | .001** | -.34 | -1.24 | .55 | .001** | .33 | -.66 | 1.34 | .50 |
| Interfere with lifestyle | 2.41 | 1.77 | 3.05 | .02* | 1.27 | .47 | 2.06 | .001** | -.17 | -1.02 | .68 | .69 |
| Pain severity at forward bending activity | 1.44 | .80 | 2.08 | .00*** | 1.23 | .74 | 1.71 | .00*** | -.81 | -1.55 | -.06 | .03* |
| Back Stiffness | 1.52 | .72 | 2.32 | .02* | .95 | .47 | 1.42 | .00*** | -.70 | -1.48 | .08 | .07 |
| Interfere with Walking | 1.16 | .70 | 1.61 | .00*** | 1.25 | .75 | 1.74 | .001** | -.13 | -.86 | .60 | .72 |
| Hurt when Walking | 1.19 | .84 | 1.53 | .01* | 1.01 | .46 | 1.56 | .001** | .10 | -.67 | .88 | .78 |
| Pain keep from standing still | .87 | .34 | 1.40 | .001** | 1.19 | .78 | 1.59 | .02* | -.06 | -.92 | .78 | .87 |
| Pain keep from twisting | 1.13 | .48 | 1.77 | .00*** | 1.13 | .78 | 1.48 | .00** | -.31 | -1.18 | .56 | .48 |
| Sit in upright hard chair | 1.41 | .80 | 2.02 | .001** | 1.45 | .96 | 1.94 | .001** | -.67 | -1.50 | .16 | .11 |
| Sit in soft arm chair | 1.34 | .82 | 1.87 | .03* | .92 | .54 | 1.29 | .04* | -.69 | -1.67 | .28 | .16 |
| Pain in lying | 1.13 | .59 | 1.66 | .00*** | 1.16 | .69 | 1.62 | .001** | -1.03 | -1.99 | -.07 | .03* |
| Pain limit normal lifestyle | 1.66 | .96 | 2.35 | .001** | 1.25 | .77 | 1.73 | .00*** | -1.22 | -2.14 | -.29 | .01* |
| Interfere with work | 1.51 | .85 | 2.16 | .01* | 1.59 | .93 | 2.24 | .001** | -.73 | -1.49 | .03 | .06 |
| Change of workplace | 1.30 | .80 | 1.79 | .001** | 1.48 | .84 | 2.12 | .001** | -.94 | -1.79 | -.09 | .03* |
| ODI | 7.00 | 4.10 | 9.89 | .001** | 8.00 | 3.42 | 12.57 | .00*** | -8.13 | -13.25 | -3.01 | .00*** |
| - | Control | McKenzie | Between group | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| m1 | 95% CI | F | p | m1 | 95% CI | F | p | F | p | Power | |||
| low up | low up | ||||||||||||
| DPQ | |||||||||||||
| Pain | 2.65 | 2.13 | 3.18 | 182.6 | .001** | 2.32 | 1.62 | 3.02 | 122.9 | .00*** | 1287.4 | .001** | 1 |
| Pain at night | 2.64 | 2.08 | 3.19 | 260.1 | .02* | 2.97 | 2.11 | 3.83 | 237.3 | .03* | 494.3 | .01* | 1 |
| Interfere with lifestyle | 2.40 | 1.90 | 2.89 | 499.5 | .03* | 2.23 | 1.50 | 2.95 | 285.1 | .02* | 732.4 | .03* | 1 |
| Pain severity at forward bending activity | 2.80 | 2.40 | 3.20 | 721.7 | .01* | 1.99 | 1.35 | 2.63 | 229.3 | .01* | 722.1 | .01* | 1 |
| Back Stiffness | 2.31 | 1.77 | 2.86 | 252.1 | .01* | 1.61 | 1.03 | 2.20 | 186.1 | .01* | 437.1 | .01* | 1 |
| Interfere with Walking | 2.08 | 1.63 | 2.52 | 333.2 | .03* | 1.95 | 1.35 | 2.54 | 298.2 | .02* | 625.9 | .02* | 1 |
| Hurt when Walking | 1.96 | 1.41 | 2.51 | 335.1 | .02* | 2.07 | 1.49 | 2.65 | 174.5 | .01* | 463.0 | .04* | 1 |
| Pain keep from standing still | 2.08 | 1.46 | 2.70 | 126.1 | .01* | 2.0 | 1.4 | 2.63 | 259.5 | .00*** | 359.4 | .001** | 1 |
| Pain keep from twisting | 2.22 | 1.64 | 2.80 | 190.4 | .04* | 1.91 | 1.23 | 2.58 | 170.2 | .03* | 474.9 | .04* | 1 |
| Sit in upright hard chair | 2.34 | 1.80 | 2.89 | 302.7 | .03* | 1.67 | 1.02 | 2.32 | 186.7 | .02* | 577.6 | .01* | 1 |
| Sit in soft arm chair | 3.31 | 2.51 | 4.10 | 257.8 | .01* | 2.61 | 2.01 | 3.21 | 351.9 | .001** | 478.5 | .01* | 1 |
| Pain in lying | 2.91 | 2.13 | 3.68 | 211.4 | .01* | 1.87 | 1.27 | 2.47 | 284.3 | .001** | 587.6 | .00*** | 1 |
| Pain limit normal lifestyle | 2.96 | 2.31 | 3.60 | 369.9 | .01* | 1.74 | 1.04 | 2.43 | 229.0 | .00** | 639.5 | .00*** | 1 |
| Interfere with work | 2.83 | 2.24 | 3.43 | 283.4 | .01* | 2.10 | 1.59 | 2.60 | 374.4 | .01* | 513.9 | .02** | 1 |
| Change of workplace | 2.68 | 1.9 | 3.37 | 212.1 | .04* | 1.17 | 1.21 | 2.25 | 321.6 | .02* | 478.5 | .04** | 1 |
| ODI | 35.5 | 27.7 | 43.3 | 213.1 | .01* | 48.9 | 41.1 | 56.7 | 107.1 | .001** | 287.5 | .01* | 1 |
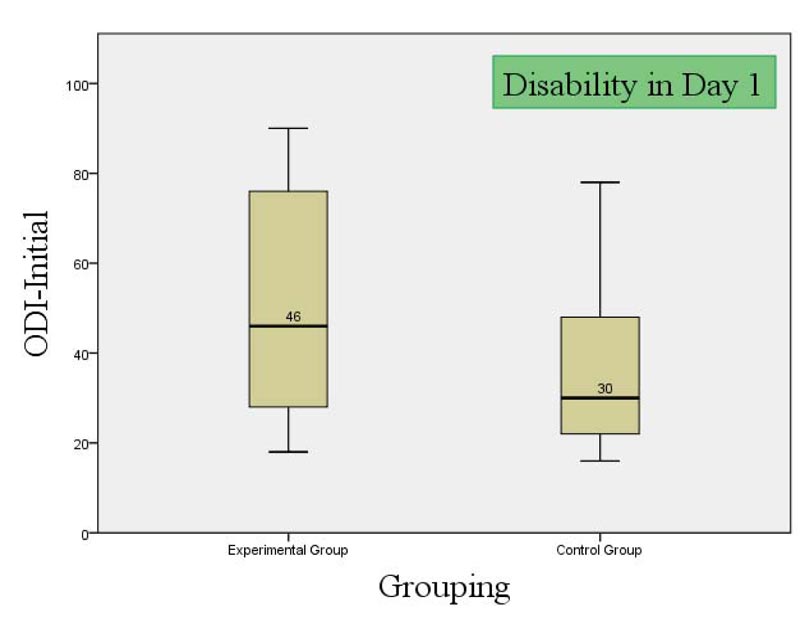
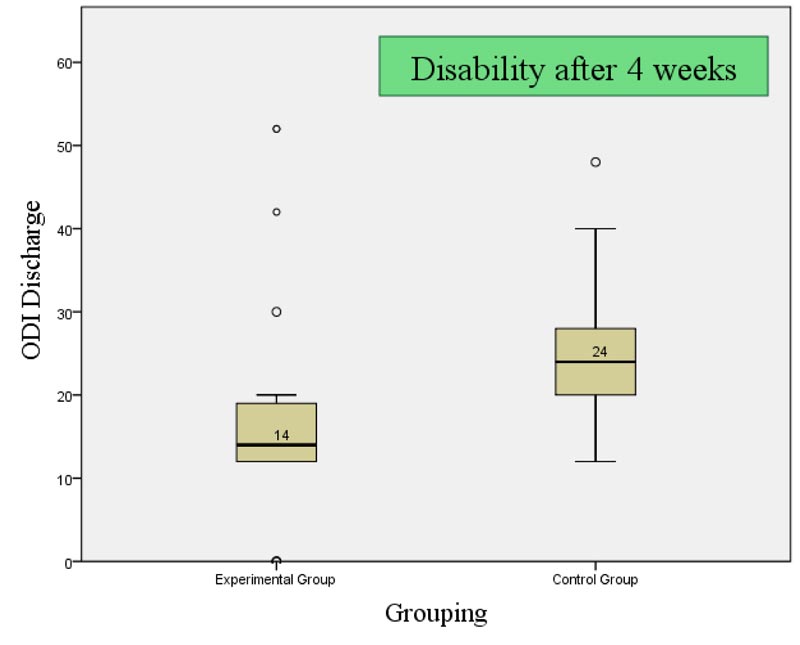
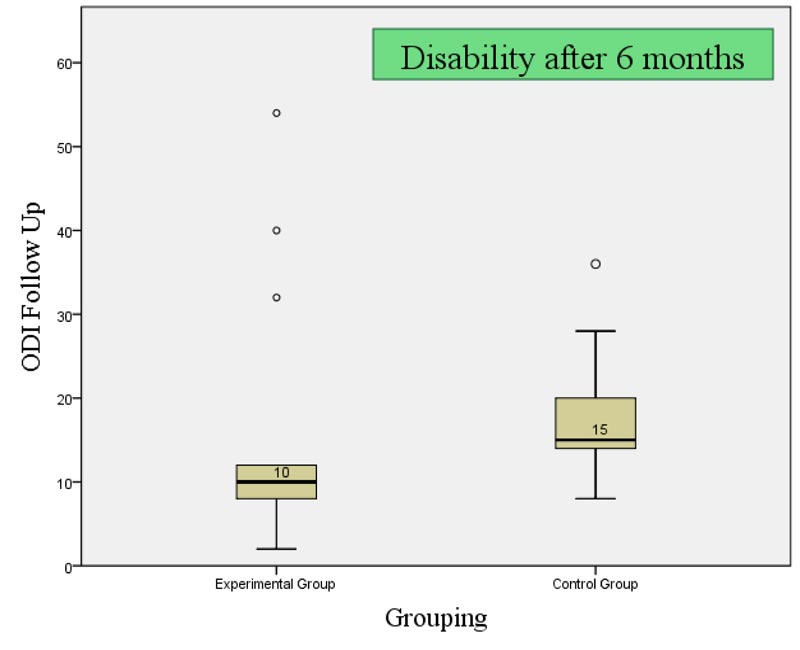
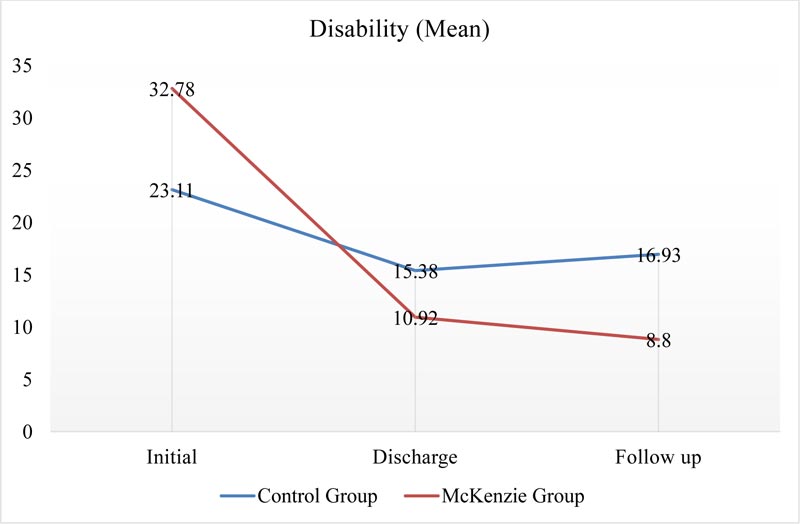
The inter-quartile range (IQR) of control in the initial, discharge and follow up (Fig. 2) was 34 (2.75, 20, 36.5), 23 (2, 18.0, 25) and 6.5 (13.5, 15, 20) and median found 30, 24 and 14 respectively. Also interquartile range (IQR) of McKenzie in initial, discharge, and follow-up was 43 (2.75, 28, 46), 13 (1, 12, 14) and 12 (0, 7, 12) and median found 46, 14 and 6 respectively. There were also notable changes of ODI mean according to the timeline in both groups and McKenzie had better remission of disability (Fig. 3).
3.6. Fear-avoidance and Bothersome in Activities from Bbaseline (day 1) to Discharge (4 weeks)
From Baseline to discharge within group analysis of Fear Avoidance Belief in physical activities, work related activities reported mean differences, lower and upper value of 95% (Table 5) as control 5.27, 3.99, 6.55 (p=.01), 5.78, 4.27, 7.30 (p=.01) and 16.3, 13.3, 19.2 (p=.01), and McKenzie 9.0, 7.96, 10.0 (p=.01), 16.7, 15.2, 18.1 (p=.00) and 36.0, 33.3, 38.6 (p=.00). “Bothersome due to Leg pain”, “abnormal sensation in leg”, “weakness in leg” and “leg pain in sitting” wasreported with a mean difference, lower and upper value of 95% (Table 3) as control 1.69, 1.31, 2.07 (p=.01), 1.63, 1.16, 2.10 (p=.000), 1.27, .690, 1.85 (p=.000) and 2.09, 1.36, 2.81 (p=.000) and McKenzie 2.16, 1.63, 2.68 (p=.01), 2.38, 1.96, 2.80 (p=.02), 2.29, 1.82, 2.75 (p=.01) and 1.38, .643, 2.13 (p=.001). The between group analysis by independent t test in FABQ reported mean difference, lower and upper value of 95% (Table 3) as -1.76, -3.70, .176 (p=.074), -5.03, -7.12, -2.94 (p=.00) and -10.1, -13.8, -6.44 (p=.01), and SBI as .12, .95, .85 (p=.7), .92, 1.6, .22 (p=.02), .631, .5, .13 (p=.3) and .49, .37, 1.1 (p=.2).
| Variables | Control | McKenzie | Between group | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| m1 | 95% CI | p | m1 | 95% CI | p | MD2 | 95% CI | p | ||||
| low | up | low | up | low | up | |||||||
| FABQ | ||||||||||||
| Physical activity | 5.27 | 3.99 | 6.55 | .01*** | 9.0 | 7.96 | 10.0 | .01*** | -1.76 | -3.70 | .176 | .074 |
| Work activity | 5.78 | 4.27 | 7.30 | .01* | 16.7 | 15.2 | 18.1 | .01* | -5.03 | -7.12 | -2.94 | .00*** |
| Total | 16.3 | 13.3 | 19.2 | .01* | 36.0 | 33.3 | 38.6 | .001** | -10.1 | -13.8 | -6.44 | .01* |
| SBI | ||||||||||||
| Leg pain | 1.69 | 1.31 | 2.07 | .01* | 2.16 | 1.63 | 2.68 | .01* | .12 | .95 | .85 | .7 |
| Sensation leg | 1.63 | 1.16 | 2.10 | .00*** | 2.38 | 1.96 | 2.80 | .02* | .92 | 1.6 | .22 | .02* |
| Weakness leg | 1.27 | .690 | 1.85 | .001** | 2.29 | 1.82 | 2.75 | .01* | .63 | 1.5 | .13 | .3 |
| Sitting leg pain | 2.09 | 1.36 | 2.81 | .001** | 1.38 | .643 | 2.13 | .001** | .49 | .37 | 1.1 | .2 |
4. DISCUSSION
This research intended to explore the effectiveness of McKenzie Manipulative Therapy for LDH patients compared with a set of conventional physiotherapy treatment. The statistical analysis showed a statistically significant difference between the two groups for the ODI, with the McKenzie group having a lower score (F=107.1)), which implies that the McKenzie group intervention was more effective in reducing disability than the control group (F=287.5, P=<.001) within the twelve treatment sessions, as well as follow up after six months. All the variables of the Dallas pain questionnaire represented a similar result. Evidence recommends [27] using similar scales to measure disability states through physiotherapy interventions.
The control and intervention groups reported similar baseline characteristics in mean age, height, and weight. The occupation among groups varied, with service holders and housewives reported for the majority of respondents. Two recent meta-analyses showed that subjects who were overweight or obese were at increased risk for both low back pain (LBP) and lumbar radicular pain [23]. Abdominal obesity is defined by waist circumference and has been associated with LBP in women [24].
As the study was conducted in the hospital setting, the priority was through the diagnosis and clinical presentations, and for concealed allocation, the groups had an insignificant similarity of baseline statistics.
Analysis of Dallas Pain Questionnaire (DPQ) and Oswestry Disability Index (ODI) has been analyzed by paired and independent t-test, and repeated measure ANOVA from baseline to discharge, discharge to follow up and baseline to follow up found a statistically significant difference in both group separately. Also, between groups analysis found McKenzie's concept to be superior in several parameters in several distinct timelines. From baseline to discharge McKenzie found better improvements in DPQ interference of lifestyle (mean difference -1.19, CI -2.4, -.33; P= <.001), Pain severity in forward bending activity (MD -.95, CI -1.88, -.02; p=<.04), Back stiffness (MD -1.19, CI -2.07, -.31; p=<.00), sit in soft armchair (MD -1.00, CI -1.99, -.012; p=<.04) and Pain limit normal lifestyle (MD -1.58, CI -2.53, -.63; p=<.001). From discharge to follow up McKenzie group was superior in DPQ Pain severity in forward bending activity (MD -.81, CI -1.55, -.06; p=<.03), Pain in lying (MD -1.03, CI -1.99, -.07; <.03), Pain limit normal lifestyle (MD -1.22, CI -2.14, -.29; <.01), Change of workplace (MD -.94, CI -1.79, -.09; p=<.03) and ODI (MD -8.13, CI -13.25, -3.01; P=<.00).
From baseline to follow-up McKenzie group shown better long term outcome in DPQ (P=<.05) with F value pain 1287.4, pain at night 494.3, interfere with lifestyle 732.4, pain severity at forward bending activity 722.1, back stiffness 437.1, interfere with walking 625.9, hurt when walking 463.0, pain from standing still 359.4, pain keep from twisting 474.9, sit in upright hard chair 577.6, sit in soft armchair 478.5, pain in lying 587.6, pain limit normal lifestyle 639.5, interfere with walking 513.9 and change of workplace 478.5 with statistical power 1. In between-group analysis, ODI had a statistical significant change with F value 287.5 (P=<.01, power 1).
However, the McKenzie group reported significantly better outcome improvement than control. The inter-quartile range (IQR) for the control was reported for the initial, discharge, and follow-up. Notable changes for the ODI mean was reported according to the timeline in both groups, with McKenzie reporting significantly better “remission of disability” than control. Several studies suggested that McKenzie therapy was more effective than most comparative treatments at short-term follow-up in comparison with the treatments included non-steroidal anti-inflammatory drugs, educational booklet, and back massage with back care advice, strength training with therapist supervision, spinal mobilization, and general mobility exercises [25]. Six studies were reviewed by Clare and colleagues [26] and 1 of the 6 groups found the comparison treatment (massage/back care advice) to be more effective on both short-term and intermediate-term disability than McKenzie therapy. No other comparative treatment was more effective than McKenzie therapy at any identified point in time. Most authors focus on short-term effects of McKenzie therapy or report outcomes within 3 months of treatment but this study creates new evidence of long-term effects also. Moreover, the study [27] showing McKenzie treatment to reduce the level of disability reaching a statistical significance at 2 and 12 months follow up.
This study holds unique features that explore changes in fear-avoidance beliefs in physical activities and work, and “impairments in different functional positions”.From Baseline to discharge within-group analysis of Fear-avoidance belief in physical activities, work-related activities and total along with “Irritability due to leg pain”, abnormal sensation in the leg, weakness in leg and leg pain in sitting by paired t-test reported mean difference, lower and upper value of 95% found significant changes in each group separately. The between-group analysis by independent t-test in FABQ and SBI reported mean difference, lower and upper value of 95% found superior results in McKenzie group in FABQ activity and total, and bothersome in abnormal sensation in the leg. In the study, the participants received controlled McKenzie manipulative therapy or a set of conventional approach weekly three days in four weeks consecutively. Similar studies explored that [28] six sessions over 3 weeks may bring benefits, as this study minimizes the length and proven increased frequency benefits the patient.
This study recruited 64 subjects with diagnosed LDH and allocated them, equally, in two groups of physiotherapy interventions and found significant differences in outcomes of DPQ, ODI, SBI, and FABQ. One comparative randomized controlled trial reported [29] with a 3-month follow-up period among 271 patients with chronic LBP two groups as the McKenzie therapy group (n = 134) and the other was electrophysical agents group, (n = 137). In 28 sessions, significant improvement was achieved like increase in spinal motion, reduction of pain and disability within both groups but the greater improvement in the McKenzie group (p <0.05) hence, this study found improvement in pain, disability, fear-avoidance, and bothersome in 12 sessions. In the mentioned study, 271 samples were recruited and revealed that the McKenzie physiotherapy with a different protocol like exercise or first-line care were significant, similar to this study with a minimum intervention time.
The study implied the appropriate randomization with limited resources and scarcity of samples. The assessor was blinded and the treatment provider had separate inclusion criteria and allocated to groups as per the randomization process. This minimalizes the potential bias and ensures masking to the patients. There was no overlap of the treatment provider, hence the intervention was a form of exercise that is difficult to blind to the intervention provider and patient. The patient’s participation was willing and voluntary. Because of Hospital-based randomization, there was variety in demographics of the patient, and in a sense despite small sample size, the result has external validity.
The limitations of this study include a smaller sample size, long duration of the study, difficulty identifying qualified subjects with a specific diagnosis for inclusion factor, supporting documents, and eligibility criteria in the timeframe of 2 years. Among the cases, 5 participants (3.4%) had a relapse with minimum central symptom within 6 months. Drop out analysis could improve the sample size but that was minimum in number so the authors don’t consider the analysis. Calculating adverse events could improve a new dimension, the study is recommended to extend to long term prospective cohort. Future studies with multicenter, compared to surgery are recommended.
CONCLUSION
The results of this study show that there is an overall statistically significant difference between the two intervention groups for the pain and disability in ODI and DPQ, but not for fear-avoidance belief and bothersome in functional activities in FABQ and SBI. This is providing insight that the McKenzie method may be more effective in addition to standard physiotherapy protocol for lumbar disc herniation.
ETHICS APPROVAL AND CONSENT TO PARTI-CIPATE
The study was approved by the CRP ethical review board (CRP R&E-0401-180). A Randomized Controlled Trial” approved by Clinical trial registry India (CTRI/2020/ 04/024667) the primary registry the authority approved by WHO trial registry.
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures were followed in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Written consent has been taken from the participants.
STANDARDS OF REPORTING
CONSORT guideline has been followed in this study.
AVAILABILITY OF DATA AND MATERIALS
The datasets generated in the current study are available from the corresponding author (Z.U.) on request.
FUNDING
None.
CONFLICT OF INTEREST
Dr. Zakir Uddin is the editorial board member of The Open Sports Sciences Journal.
ACKNOWLEDGEMENTS
The authors acknowledge Imtiaze Ahmed and Maria Shikder for the data collection and Md. Shahoriar Ahmed and Rubayet Shafin for supporting the analysis of data.


