All published articles of this journal are available on ScienceDirect.
Immediate Effects of Pencil Push-Up Exercise on Visual Accommodation Skills in Amateur Badminton Players: A Randomized Controlled Trial
Abstract
Background
Visual skills are crucial for peak athletic performance, with Visual Accommodation (VA) playing a vital role. However, the immediate effects of interventions on VA in sports remain unclear.
Objective
To investigate the acute effects of a 10-minute Pencil Push-Up (PPU) exercise on VA skills in amateur badminton players.
Methods
A two-arm, parallel, randomized controlled trial was conducted with twenty-eight amateur badminton players. Participants were matched by age, duration, and frequency of badminton practice, as well as visual health, and randomly assigned to either a Trained Group (TG) or an untrained group (NT). The TG performed a 10-minute PPU exercise, while the NT rested with closed eyes for the same duration. VA parameters, including Amplitude of Accommodation (AA), Accommodative Facility (AF), and Near Point of Convergence (NPC), were assessed before and after the intervention.
Results
Significant improvements in AA and AF were observed in the TG from pre- to post-intervention (AA: p < .0001, Cohen's d = 1.68; AF: p < .0001, Cohen's d = 3.10). However, no significant changes were observed in NPC (p= .45, Cohen's d =0.60). Furthermore, the TG exhibited greater improvements in AA and AF compared to the NT at post-intervention (AA: 95%CI= [-2.812 to -0.2314], p = .02; AF: 95%CI= [-8.363 to -3.680], p < .0001). No changes were observed in the NT group.
Conclusion
A single session of pencil push-up exercise acutely enhanced visual accommodation skills, specifically amplitude of accommodation and accommodative facility, in amateur badminton players. This suggests that visual accommodation training methods like pencil push-ups could improve visual performance in sports.
1. INTRODUCTION
In elite sports, perceptual-cognitive vision skills (e.g., visual accommodation, binocular vision, depth perception, visual acuity, and visual reaction time) play a significant role in an athlete’s capacity to achieve peak performance [1]. Visual Accommodation (VA), one of these key visual skills, is a process that allows the eye to focus on an object with good depth perception as its distance varies [2, 3]. A range of metrics, such as the Amplitude of Accommodation (AA), Near Point of Convergence (NPC), and Accommodative Facility (AF), can be used to analyze the VA system. The AF refers to the speed of the eye’s capacity to change focus from one distance to another. It is described as a process in which the ocular system changes its refractive power to bring images at different distances into focus by altering the shape of the elastic lens via the ciliary body [4]. In contrast, the NPC plays a critical role in visual attention when objects approach from varying distances [5] and is a common binocular vision deficit after a sport-related concussion [6]. The AA works as a reflex, shifting the eyes’ focus from the greatest distance (far point) to the lowest distance (near point) for a clear image; therefore, poor accommodative facility affects the perception of depth and visual processing speeds [7]. Studies such as those by Redondo et al. [8-10] and Vera et al. [11, 12] have highlighted various factors influencing VA, such as caffeine intake [8], diurnal variations, task-relevant stimuli [10], attention [9], placebo and nocebo effects [11], and exercise intensity [12], providing valuable insights into the complexity of visual function.
In recent years, sports vision training has gained increasing attention from coaches and sports organizations as a way to help athletes reach peak levels of performance. Sports vision training focuses on strengthening an athlete’s visual abilities within their sport-specific setting. This training elicits communication between the visual and the brain’s proprioceptive systems, which is vital during the execution of sports skills [13-15]. Previous studies have reported the effectiveness of vision training programs on athletic performance, especially in racquet sports [16-18]. For instance, Karimian et al. [16] improved visual and sports performance in female badminton players after a 10-session training program targeting vergence facility, accommodative facility, and hand-eye coordination. Similarly, Bonato et al. [17] reported improved competitive performance in tennis players who underwent 12 weeks of visual training. Additionally, Hülsdünker et al. [18] found that stroboscopic training improved visuomotor performance and visual perception speed in high-level badminton players after four weeks of training. However, Strainchamps et al. [19] showed contrasting results. They showed that table tennis athletes who underwent a 10-minute table tennis-specific warmup with stroboscopic eyewear did not experience any significant improvement in reaction speed compared to a warmup under normal visual conditions.
VA training using Pencil Push-Up exercises (PPU) is an established and effective treatment that is commonly used for patients presenting with eye convergence insufficiency [20-22]. Sapkota et al. [21] evaluated 84 patients with convergence insufficiency over six weeks of eye workout programs utilizing PPU and found that 10 minutes of training enhanced NPC and alleviated symptoms of convergence insufficiency patients. Moreover, Hazman et al. [23] found that 10 minutes of PPU could improve AA, AF, and the corresponding accommodation system in healthy young adults. These findings [21-23] suggest that PPU can effectively train the eye's convergence and accommodation systems, which are crucial for maintaining clear vision at varying distances.
In the context of badminton, where athletes constantly need to focus on objects at different distances, including the shuttlecock, opponents, and various parts of the court, strong visual skills are essential for optimal performance. Players must quickly adjust their focus from far distances to near ones, which can be particularly challenging during rapid movements and high-speed gameplay [10]. This unique visual demand in badminton highlights the potential benefits of interventions like PPU, which specifically target and improve visual accommodation skills. Despite the critical role of visual skills in badminton performance, few studies have explored the effectiveness of visual training interventions specifically tailored to badminton players [16, 18, 24, 25]. Moreover, existing research has yet to investigate the impact of a single-session PPU exercise on VA in the context of badminton.
To that end, the present investigation sought to examine the acute effects of a 10-minute PPU exercise on the VA skills of amateur badminton players. Furthermore, the outcomes of this study may have broader implications for athletes in other sports, as well as individuals with similar visual demands in various occupational or recreational activities.
2. METHODS
2.1. Participants
This study calculated sample size estimates from a previous study [26] using G*Power 3.1.9.2 analysis (effect size: f = 0.7, alpha = 0.05, power = 0.8, critical F = 4.07, Lambda = 23.52). The calculated sample size was 24 plus 4 for 20% dropout, so the final sample size of 28 participants (14 participants for each group) was needed (Supplementary material).
A two-arm, parallel, randomized controlled trial was conducted to assess the acute effects of a 10-minute PPU on visual accommodation skills in amateur badminton players. Twenty-eight participants (12 males and 18 females) with an average age of 22 ± 2 years, height of 167 ± 8 cm, body mass of 55.3 ± 7.9 kg, and body mass index of 20 ± 1 kg·m2 (mean ± SD) were recruited from local badminton clubs and organizations affiliated with Rangsit University in Thailand. The study was carried out between 2021 and 2022. During recruitment, participants had to meet the following criteria included: 1) be active members of a university badminton club, 2) regularly engaged in badminton practice for a minimum of 3 hours per day and 3 days per week, 3) not pursuing badminton as a professional career, 4) no prior exposure to similar visual training interventions, 5) best corrected monocular visual acuity with a contact lens of 20/25 or better at far and near using the Snellen chart at 6 meters for far distance and reduced Snellen charts at 14 inches for near distance, 6) no history or presence of the following conditions diagnosed by an optometrist such as strabismus (constant misalignment of the eyes), amblyopia (lazy eye), refractive surgery (e.g., LASIK), manifest or latent nystagmus (involuntary eye movements), and 7) no history of any systemic diseases known to affect vision, such as brain injury or neurological disorders impacting vision and movement. Additionally, other inclusion criteria, such as visual acuity and absence of ocular diseases or systemic conditions affecting eyesight, were verified through comprehensive eye examinations conducted by trained optometrists. Participants underwent visual screening using standardized protocols to assess visual acuity and refractive error, and any abnormalities or deviations from the inclusion criteria were noted and addressed accordingly. All participants provided written informed consent after explaining the experimental procedures and the potential risks and benefits of the study. Ethical approval was obtained from Mahidol University (MU-CIRB 2021/140.2203), and the study protocol and procedures conformed to the 2013 Declaration of Helsinki.
2.2. Study Design
First visit: 24 hours before visiting the laboratory, participants were instructed to abstain from alcohol and caffeine and sleep for at least eight hours. Upon arrival, their height and weight were measured using a stadiometer and a digital weighing scale. Body Mass Index (BMI) was calculated using the formula: body weight (kg) divided by the square of height (m2). Participants were matched by age range (age:22 ± 2 years), duration and frequency of badminton practice (3±1 hours per day and 3±1 day weekly), and visual health and randomly assigned to either a trained group (TG, n=14) or an untrained group (NT, n=14) using a computer-generated randomization program. Neither participants nor researchers knew the group assignments beforehand.
Second visit: On the training day, participants returned to the laboratory at 7 a.m. for the assigned intervention (PPU or rest) for 10 minutes. The TG group performed a 10-minute pencil push-up exercise, whereas the NT group rested in a chair with their eyes closed for 10 minutes. A different optometrist, blinded to group allocation, assessed all visual acuity parameters before and after the intervention to minimize bias.
2.3. Measurements
2.3.1. Visual Screening
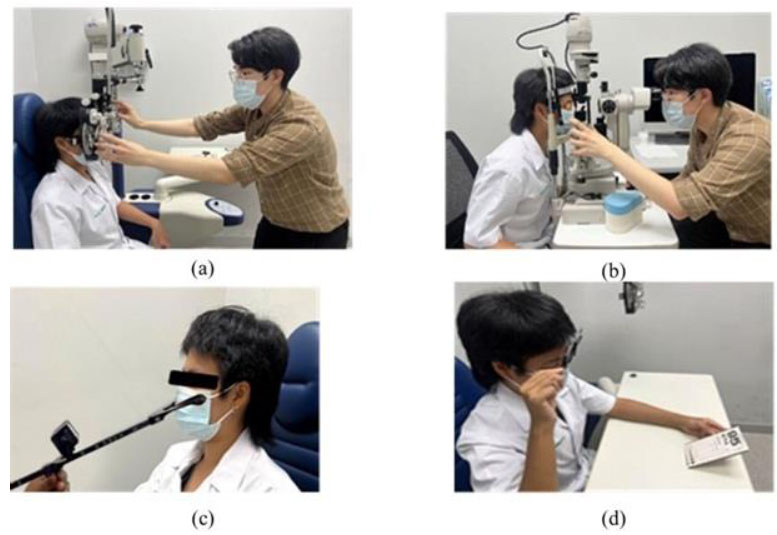
An optometrist screened individual participants for eye values (Figs. 1a and 1b). During the recruitment process, the visual acuity (in decimal), both proximal and distal, and the refractive error of the eyes (OD) (in diopter) of the eyes were assessed. Fogging technique [27] was used to ensure that the participant’s eyes were unaccommodated during pre-data collection and before training.
2.3.2. Parameters for Pre- and Post-data Collection
2.3.2.1. Amplitude of Accommodation (AA) Assessment
The Royal Air Force (RAF) near-point rule (Fig. 1c), the eye's best-corrected vision, was used to measure AA [28]. The RAF rule had good (ICC=0.952) test-retest reliability [29]. The reduced Snellen chart at visual acuity 20/25 was steadily pushed closer to the participant until a continuous blur was observed. The measurement was then conducted three times, and the average (in centimeters) was used for data analysis by converting to Diopters (D). The average reading of the right eye was recorded in diopters.
2.3.2.2. Accommodative Facility (AF) Assessment
Binocular AF (BAF) was assessed by measuring cycles of shifts per minute between two levels of accommodation (e.g., +2 D vs. −2 D). The BAF test had a good (ICC= 0.95 to 0.98) test-retest reliability [30]. This test was performed at a distance of 40 cm and binocularly for one minute utilizing a reduced Snellen chart card with a text size of 20/30 and a ±2.00 D lens flipper (Fig. 1d). Once the lens flipper is placed in front of the participant’s eyes, the participants must clear the letters as quickly as possible. The number of complete “flips” that the participants clear in one minute determines the outcome of the test. The capacity of AF was assessed in cycles per minute.
2.3.2.3. Near Point of Convergence (NPC) Assessment
Binocular NPC assessment is similar to measuring the AA but with a dot on a line chart as the target [31]. The test had a high sensitivity (94.4%) and specificity (83.3%) to identify convergence insufficiency in young adults [32]. The researcher asked the participants to focus on a single black dot target and slowly move toward their eyes at a constant and linear rate. If a single target appears double, the participants must be informed. This value was noted in centimeters (cm). The average value was taken from three measurements.
2.4. Training program
The 10-minute VA training program using a pencil push-up exercise is displayed in Fig. (2). Briefly, participants held one pencil at arm's length in front of them, bringing it slowly and steadily up to the nose while keeping the pencil's tip concentrated and visually single. The pencil tip started to blur when it was very close to the nose, as long as it was still single and there were no two pencil tips visible. When the pencil doubled, the participants made a concerted effort to observe it as a single object. At that point, the participants were instructed to relax while keeping it single and holding this position for two seconds. If the participant could not keep the pencil tip single, they returned it to arm's length and began the procedure again. This process was repeated for 10 minutes, and then the participant rested their eyes for one minute by gazing at the distance.
In the logbook, the rate of treatment compliance and dropout to the intervention, as well as safety were assessed through direct observation by trained research assistants and self-reporting by participants.
2.5. Data Analysis
Participants’ general characteristics are presented as mean ± standard deviation. The Shapiro-Wilk test revealed that the data were normally distributed. All variables were analyzed using repeated measures Analyses of Variance (ANOVA) with one between-groups factor (with two levels, i.e., TG and NT groups) and one within-group factor (with two levels, i.e., pre-and post-test). When a significant F-ratio was obtained, post hoc analysis with Bonferroni adjustment was used to identify the pair of mean values that showed significant changes. Data are presented as mean ± standard error of the mean. Differences (F value), effect size partial eta-square (ηp2), and significance (p) are shown. To account for differences from the pre-test, the values of percentage change (%∆) were calculated using the formula: [(post- minus pre-test) and divided by pre-test] multiplied by 100. The differences in %∆ between the two conditions were analyzed using an independent t-test. Cohen's d and 95%CI were also calculated to determine effect sizes to compare means between conditions. Statistical significance was set at p < .05. All statistical analyses were performed using SPSS version 20.

| Variable | TG n=14 |
NT n=14 |
p-value |
|---|---|---|---|
| Age (Year) | 22±2 | 24±1 | ns |
| Height (cm) | 167±8 | 161±6 | ns |
| Sex (Male: Female) | 6:8 | 4:10 | - |
| BW (kg) | 55.3±7.9 | 50.9±6.4 | ns |
| BMI (kg/m2) | 19.8±1.1 | 19.5±1.3 | ns |
| Number of hours spent playing badminton per day | 3±1 | 3±1 | ns |
| Number of days spent playing badminton per week | 4±1 | 4±1 | ns |
| Visual Acuity (Right) (Decimal) | 0.9±0.1 | 1.0±0.0 | ns |
| Visual Acuity (Left) (Decimal) | 0.9±0.1 | 1.0±0.0 | ns |
| Visual Acuity (Both eyes) (Decimal) | 0.9±0.1 | 1.0±0.0 | ns |
| Refractive error (Right) (Diopter) | -0.75±1.25 | -0.75±1.00 | ns |
| Refractive error (Left) (Diopter) | -1.00±1.25 | -0.50±1.00 | ns |
3. RESULTS
The general characteristics of the participants are presented in Table 1. There was no difference in the parameters between the TG and NT groups (p>.05).
In the TG group, there was a significant effect of time (pre- and post-test) on AA after 10-minute PPU training (F (1,26) = 19.63; ηp2= .43; p = .0002), with a significant increase observed (95%CI= [2.399 to 4.530], p < .0001). Conversely, there were no significant changes in AA values from baseline in the NT group (95%CI= [-0.4085 to 1.723], p > .31). Additionally, statistically significant differences between the TG and NT groups in AA at the post-test were detected (95%CI= [-2.812 to -0.2314], p = .02). The percentage change (%∆) indicated greater improvement in AA for the TG group compared to the NT group post-training (TG: 44±6%, NT: 8±4%, Cohen's d = 1.68, 95%CI= [-51.30 to -20.41], p < .0001).
For AF, there was a significant effect of time (pre- and post-test) and groups (F (1,26) = 108.2; ηp2= .81; p < .001). A significant improvement post-PPU was shown in the TG group (95%CI= [6.650 to 9.050], p < .0001), while no changes were observed in the NT group (95%CI= [-0.7716 to 1.629], p = .81). Comparing the TG and NT groups post-test, the TG group had a significantly greater AF value (95%CI= [-8.363 to -3.680], p < .0001) (Table 2). The %∆ indicated greater improvement in AF for the TG group compared to the NT group post-training (TG: 57+7%, NT: 3+2%, Cohen's d = 3.10, 95% CI= [-69.9 to -40.6], p < .0001) (Fig. 3).
Regarding NPC, there were no significant effects of time (pre- and post-test) and groups (TG and NT) (F (1,26) = .32; ηp2= .01; p = .57 post-PPU exercise. No difference in NPC values was observed between the TG and NT groups post-training (TG: 95%CI= [-0.6085 to 0.5656], p > .99 and NT: 95%CI= [-0.4085 to 0.7656], p = .95) (Table 2). The %∆ indicated no difference in NPC post-training between the TG and NT groups (the TG = 3±4%, the NT = 2±2%, Cohen's d = 0.04, 95%CI= [-8.54 to 9.54], p = .45) (Fig. 3).
| Groups | Parameter | Pre-test | Post-test | Significance of Main Effects p-value |
|
|---|---|---|---|---|---|
| Within-group | Between Groups | ||||
| TG | AA (Diopter) |
7.94 ± 0.22 | 11.41±0.59*, # | <.0001* | .02# |
| NT | 9.23±0.26 | 9.89±0.39 | ns | ||
| TG | AF (Cycle/minute) |
14.25 ± 0.72 | 22.10±0.63*, # | <.0001 * | <.0001# |
| NT | 15.65 ± 0.79 | 16.08±0.73 | ns | ||
| TG | NPC (centimeter) |
8.5 ±0.5 | 8.4±0.3 | ns | ns |
| NT | 8.4± 0.2 | 8.6±0.2 | ns | ||
*p<.05 Significant between Pre- and Post-training.
#p<.05 Significant between trained and untrained groups at the post-test.

a Significant between trained and untrained groups at p<0.05.
The treatment compliance rate was satisfactory, with no instances of dropout observed. Additionally, the absence of adverse effects underscores the safety and feasibility of the intervention protocol used in our study.
4. DISCUSSION
The main finding of the present study was that 10 minutes of pencil push-up exercise improved visual accommodation skills by increasing the values of AA and AF. Furthermore, percentage changes from pre-to post-test improved in AA and AF but not NPC in the TG group compared to the NT group.
For visual screening, the results demonstrated that all participants had normal visual acuity values (~ 0.9 Decimal for both eyes) and refractive error (~ -0.75 Diopter for both eyes). For data on the VA system, mean values for AA, AF, and NPC have been previously obtained [33-35]. Semedo et al. reported that the value of AA usually declines with age, and the mean value of AA is about 15.33 Diopter in 11-year-olds and about 10.40 Diopter in 17-year-olds. Whereas the mean value of AF in the normal eyesight group was 15.6 Cycles Per Minute (CPM) [34], and the mean value of NPC was 9.92 cm at 18–20 years of age and progressively increased with age [35]. Compared data from this study to the previous reports, participants in both groups at baseline had the average range values for monocular AA (right eyes). However, it appeared lower in the TG (9.23±0.26 Diopter). The average values of AF fell within a normal range in both groups (TG=14.25 ± 0.72 CPM and NT=15.65 ± 0.79 CPM), and NPC seemed a bit higher than normal (TG=13.39 ± 0.53 cm and NT=10.05 ± 0.46 cm). For baseline observations, data indicate that participants had normal eye function and similar values of VA in both groups before starting the training intervention.
The present study performed the test for AA only in the dominant eye (Monocular) of all subjects, whereas NPC and AF were assessed when both eyes worked together (Binocular). Binocular NPC indicates the eye's function of convergence, whereas binocular AF indicates how well the eye's function of accommodation and convergence worked together [4, 5, 7]. The present results demonstrate the immediate effects of the PPU exercise, as the TG group achieved significantly higher values only for monocular AA and binocular AF than the NT group. In many professional sports, enhanced visual function combined with strong perceptual-cognitive abilities can give athletes a competitive advantage. Even though it is well documented that PTT is an efficient home-based therapy for patients with VA insufficiency [20, 22, 33], in this study, PPU exercise was utilized in badminton players, which aimed to improve VA on-court. PPU involves repetitive stimulation and relaxation of the eye's accommodation processes, leading to improved flexibility and responsiveness of the eye muscles. For practicing, the players slowly moved the pencil toward their nose and then away from their nose while keeping their eyes on the tip of the pencil with a single and clear vision throughout the training. This procedure was repeatedly performed for 10 minutes. Therefore, an improvement in AA and AF would be explained by the fact that when the eye’s accommodation processes are stimulated and relaxed repeatedly, this might cause eye muscles to be more flexible and faster to respond to stimuli [22] and result in an improvement in accommodation abilities [20]. The VA skills are also linked to important perceptual-cognitive processes of the brain, which influence how quickly athletes can make decisions and execute skills [36]. Additionally, our study did not observe significant enhancements in the percentage changes of NPC following the training session. This finding contrasts with previous research conducted by Sapkota et al. [21], which reported NPC improvement after 6 weeks of pencil push-up therapy in patients with Convergence Insufficiency (CI). It's worth noting that our study participants were healthy individuals, whereas Sapkota et al. focused on patients with CI, potentially contributing to the differing outcomes.
For practical implication, our study sheds light on the potential role of VA training using PPU in injury prevention strategies for badminton players. By enhancing perceptual-cognitive skills, such as spatial awareness and depth perception, targeted visual training interventions may aid in injury mitigation on the court. This aligns with previous research highlighting the importance of vision training in reducing injury risk in sports [37, 38].
Limitations should be noted in this study. Firstly, the relatively small sample size may not be representative of the characteristics of the broader population of badminton players. Secondly, while a training effect was observed, establishing whether there was a transfer effect remains challenging. Future research could enhance the study design by incorporating additional eye tests to determine 'near transfer' and possibly include badminton perceptual-cognitive/vision skill tests, such as badminton-specific skills, hand-eye coordination, or reaction time, to assess any 'far transfer' to sports performance. Thirdly, the absence of retention tests in the experimental protocol limits our understanding of the durability of post-experimental effects over time. Including retention tests would have provided further insight into the persistence of the observed improvements in visual acuity following the intervention. Fourthly, this study focused on short-term training, which restricts the generalizability of the findings to long-term benefits and their potential implications for on-court performance. Fifthly, the real-time limitations faced by the researcher, such as the COVID-19 situation and resource limitations, may have impacted the scope and depth of the study. Finally, since this study only tested binocular AF, the improvement in AF cannot discern whether it resulted from an increase in AA or NPC. Further research should measure both monocular and binocular AF to elucidate these mechanisms.
CONCLUSION
In conclusion, our study demonstrates that a brief 10-minute eye training session using pencil push-up exercises leads to acute improvements in amplitude of accom modation, and accommodative facility among badminton players compared to the untrained group. These findings suggest the potential benefits of incorporating visual training programs, such as pencil-push-up exercises, to enhance visual accommodation skills in badminton players. However, further research is needed to explore the long-term sustainability of these improvements and their translation to on-court performance.
AUTHORS' CONTRIBUTIONS
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| AA | = Amplitude of Accommodation |
| AF | = Accommodative Facility |
| BAF | = Binocular Accommodative Facility |
| BMI | = Body Mass Index |
| ICC | = Intraclass Correlation Coefficient |
| NPC | = Near Point of Convergence |
| NT | = Untrained Group |
| ηp² | = Partial Eta-square |
| D | = Diopters |
| PPU | = Pencil Push-Up |
| RAF | = Royal Air Force |
| TG | = Trained Group |
| VA | = Visual Accommodation |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval was obtained from Mahidol University (MU-CIRB 2021/140.2203).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
All participants provided written informed consent after the experimental procedures, potential risks and benefits of the study were explained.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available from the corresponding author, [A.A] on special request.


